Maternal mortality in the U.S. remains a pressing public health crisis, with the country leading its high-income peers in pregnancy-related deaths. Alarmingly, over 80 percent of these deaths are preventable, highlighting a dire need for enhanced maternal health strategies. Recent studies indicate that between 2018 and 2022, maternal mortality rates have risen, revealing stark disparities influenced by race, state, and healthcare access. The implications of inadequate postpartum care and systemic healthcare disparities continue to affect vulnerable populations, most notably among American Indian, Alaska Native, and non-Hispanic Black women who face significantly higher risks. With cardiovascular disease emerging as a leading cause of death during pregnancy, it becomes clear that comprehensive reform is essential to safeguard maternal well-being throughout gestation and beyond.
In recent years, the issue of maternal mortality in the U.S. has garnered increasing attention as pregnancy-related fatalities show alarming trends. The rising challenges in managing maternity care and ensuring adequate postpartum support reveal vital gaps in health services. Throughout various demographics, disparities linked to race and state have magnified, suggesting that biases within the healthcare landscape adversely affect maternal health outcomes. Not only do systemic inequities contribute to heightened risks, but chronic conditions like cardiovascular disease are also becoming prevalent among expectant mothers. Addressing these critical elements not only requires an overhaul of healthcare policies but also calls for increased awareness and targeted interventions to improve maternal health across the nation.
The Alarming Rise of Maternal Mortality in the U.S.
Maternal mortality in the U.S. remains a critical public health concern, as evidenced by the disturbing statistics highlighting the rise in pregnancy-related deaths. Between 2018 and 2022, the country recorded an alarming increase in maternal mortality rates, with data revealing that the U.S. leads other high-income nations in this area. This trend underscores serious flaws in the healthcare system, including inadequate prenatal and postpartum care and systemic inequities that disproportionately affect marginalized racial and ethnic communities. Given that over 80% of these deaths are deemed preventable, the pressing need for systemic reform in maternal healthcare cannot be overstated.
The significant variations in maternal mortality rates across states further illustrate the problem. For instance, American Indian and Alaska Native women face nearly four times the risk of pregnancy-related death compared to white women, highlighting stark healthcare disparities. This discrepancy necessitates a reevaluation of healthcare policies, practices, and access, as many women still encounter barriers to receiving adequate and timely care during pregnancy and afterward. Addressing these disparities is crucial not only for improving maternal health outcomes but also for ensuring equitable healthcare access across all populations.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
The leading causes of maternal mortality in the U.S. include cardiovascular disease, hemorrhage, and complications from chronic conditions. Cardiovascular disease alone accounts for over 20% of pregnancy-related deaths, highlighting the increasing prevalence of conditions like hypertension among pregnant individuals.
How does maternal mortality in the U.S. compare to other high-income countries?
The U.S. has the highest rate of maternal mortality among high-income countries, with over 80% of pregnancy-related deaths deemed preventable. The significant disparities are attributed to a fragmented healthcare system, inequitable access to care, and systemic biases affecting marginalized racial and ethnic groups.
What impact does postpartum care have on maternal mortality in the U.S.?
Postpartum care is crucial as nearly a third of maternal deaths occur between 42 days and one year after pregnancy. Improving postpartum healthcare systems can significantly reduce maternal mortality by providing ongoing support and monitoring for women during this critical recovery period.
What strategies can reduce healthcare disparities in maternal health?
To reduce healthcare disparities in maternal health, targeted policies are necessary to address inequities in access to care, enhance community resources, and ensure that care providers are trained to recognize and address biases that affect how care is delivered.
What role does cardiovascular disease play in pregnancy-related deaths?
Cardiovascular disease is a leading cause of maternal mortality, accounting for significant fatalities among pregnant individuals. The rise in chronic hypertension among younger people suggests a shift in risk factors, necessitating increased awareness and better management strategies during pregnancy.
Why are late maternal deaths important in the context of maternal mortality rates?
Late maternal deaths, which occur from 42 days to one year post-pregnancy, represent a significant portion of maternal mortality and underscore the need for continuous postpartum care. Recognizing this period can lead to better healthcare policies that support ongoing recovery and monitoring.
How can tracking and reporting of maternal mortality in the U.S. be improved?
Improvements in tracking maternal mortality can be achieved by enhancing the data collection process, such as ensuring that all states accurately report pregnancy-related information on death certificates and investing in public health infrastructure to monitor these deaths consistently.
What are the implications of rising maternal mortality rates during the COVID-19 pandemic?
The rise in maternal mortality rates during the COVID-19 pandemic highlights vulnerabilities in maternal healthcare systems, with increased deaths due to delays in care and exacerbation of existing health disparities. This situation calls for urgent policy reviews and healthcare improvements to prevent future increases.
| Key Points | Details |
|---|---|
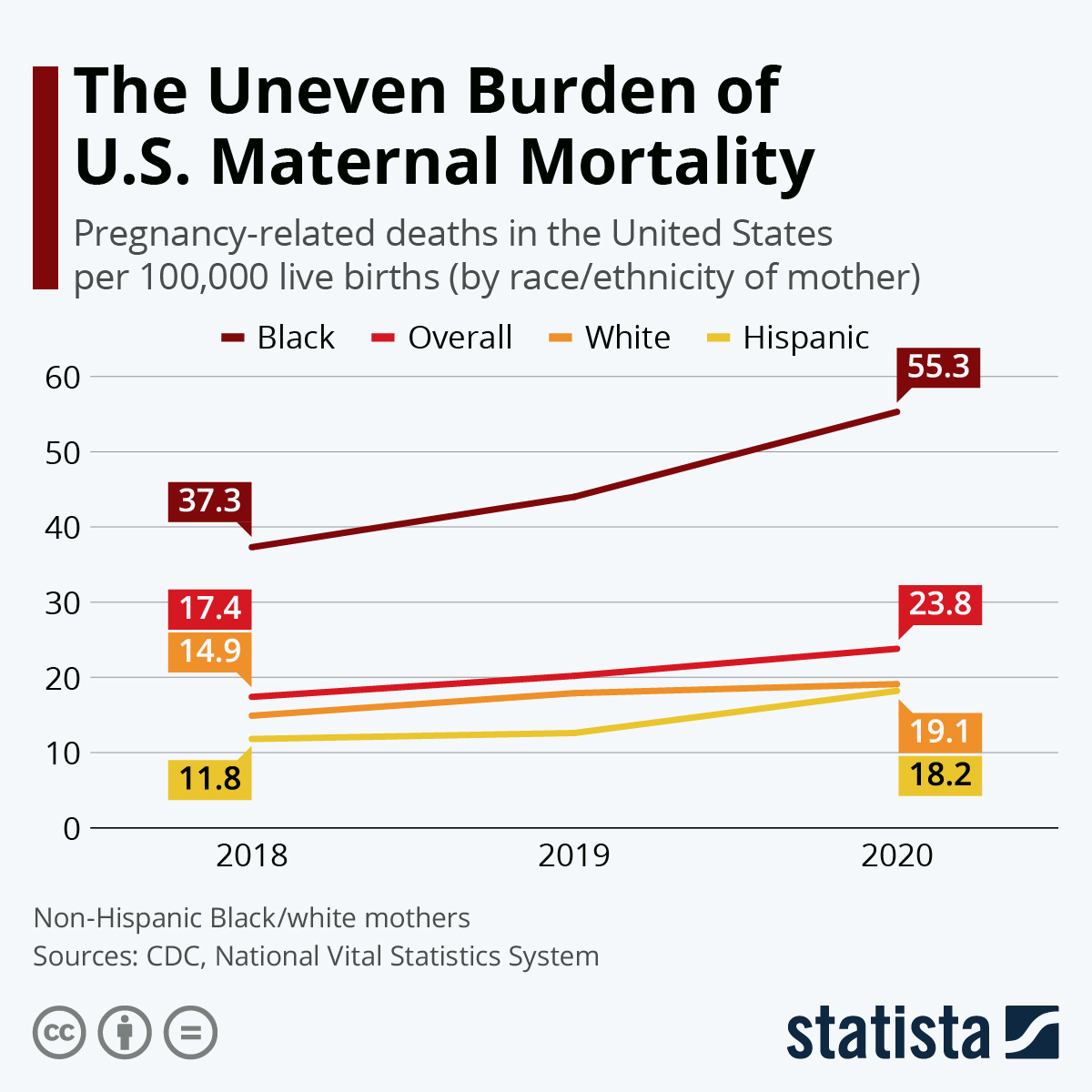
| Rising Maternal Mortality | The U.S. has the highest maternal mortality rate among high-income countries, which has increased from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. |
| Preventability | More than 80% of pregnancy-related deaths in the U.S. are preventable. |
| Racial Disparities | American Indian and Alaska Native women face the highest mortality rates at 106.3 per 100,000, followed by non-Hispanic Black women (76.9) and white women (27.6). |
| Impact of Chronic Conditions | Cardiovascular disease has become the leading cause of pregnancy-related deaths, particularly impacting younger age groups (25-39). |
| Postpartum Care | Late maternal deaths (after 42 days postpartum) account for nearly a third of pregnancy-related deaths, indicating a need for better postpartum care. |
| Need for Policy Changes | Addressing state-level disparities and investing in public health infrastructure is essential for improving maternal health outcomes. |
Summary
Maternal mortality in the U.S. is a critical public health issue that continues to trend in the wrong direction despite evidence that many of these deaths can be prevented. With a maternal mortality rate significantly higher than other high-income countries, it is vital for the U.S. to implement better prenatal and extended postpartum care strategies. There is a clear need to address the racial disparities in these rates, with particular attention to the alarming statistics affecting marginalized communities. Overall, effective policy changes, increased funding for healthcare initiatives, and improvements in care quality are essential measures to reduce maternal mortality and ensure better health for all mothers in the country.