AI in pediatric cancer prediction is revolutionizing the way physicians approach the management of brain tumors in children, particularly gliomas. Recent studies show that AI tools can analyze multiple magnetic resonance imaging (MRI) scans over time to predict relapse risks with remarkable accuracy, surpassing traditional methods. For instance, the application of machine learning cancer techniques has demonstrated up to 89% accuracy in predicting the recurrence of gliomas within a year post-treatment. By leveraging advanced approaches like MRI temporal learning, these AI models are transforming our understanding of pediatric cancer dynamics. As a result, we are witnessing a shift towards more personalized and informed treatment plans that could significantly enhance patient care and outcomes in pediatric oncology.
Artificial intelligence in predicting pediatric cancer recurrence is a groundbreaking development in the field of pediatric oncology. This innovative application of technology, often referred to as pediatric cancer AI, utilizes advanced algorithms to forecast the likelihood of tumor relapse, particularly in cases involving brain-related malignancies. Through methods such as glioma recurrence prediction, researchers are honing in on the capacities of machine learning cancer models to analyze sequential MRI images, providing deeper insights into patient conditions. The utilization of MRI temporal learning further refines these forecasts by integrating a timeline of imaging data to better assess changes in tumor behavior. Embracing these technological advancements allows for more proactive strategies in managing brain cancer, ultimately aiming to improve treatment efficacy and patient quality of life.
Understanding the Impact of AI in Pediatric Cancer Prediction
Artificial Intelligence (AI) is revolutionizing the landscape of pediatric cancer prediction, particularly when it comes to the analysis of brain tumors like gliomas. Traditionally, predicting the risk of cancer recurrence has relied on less accurate methods, but with advancements in AI technologies, the potential for significantly improved outcomes is becoming clearer. Research conducted by Mass General Brigham demonstrated that AI tools could analyze vast datasets of MRI scans over time, offering a predictive accuracy that far surpasses conventional techniques. This shift means that clinicians can potentially identify patients at a higher risk for relapse earlier than ever before, leading to more personalized treatment plans.
The study conducted at Mass General Brigham highlights the importance of using AI not only for enhanced accuracy but also for alleviating the burden of recurring imaging procedures on pediatric patients. Frequent follow-ups with MRI scans can be a source of stress for both children and their families. With AI in pediatric cancer prediction, doctors may soon be able to determine which patients can reduce follow-up frequency safely, sparing them unnecessary imaging while still closely monitoring their health.
Advancements in Machine Learning for Cancer Recurrence Prediction
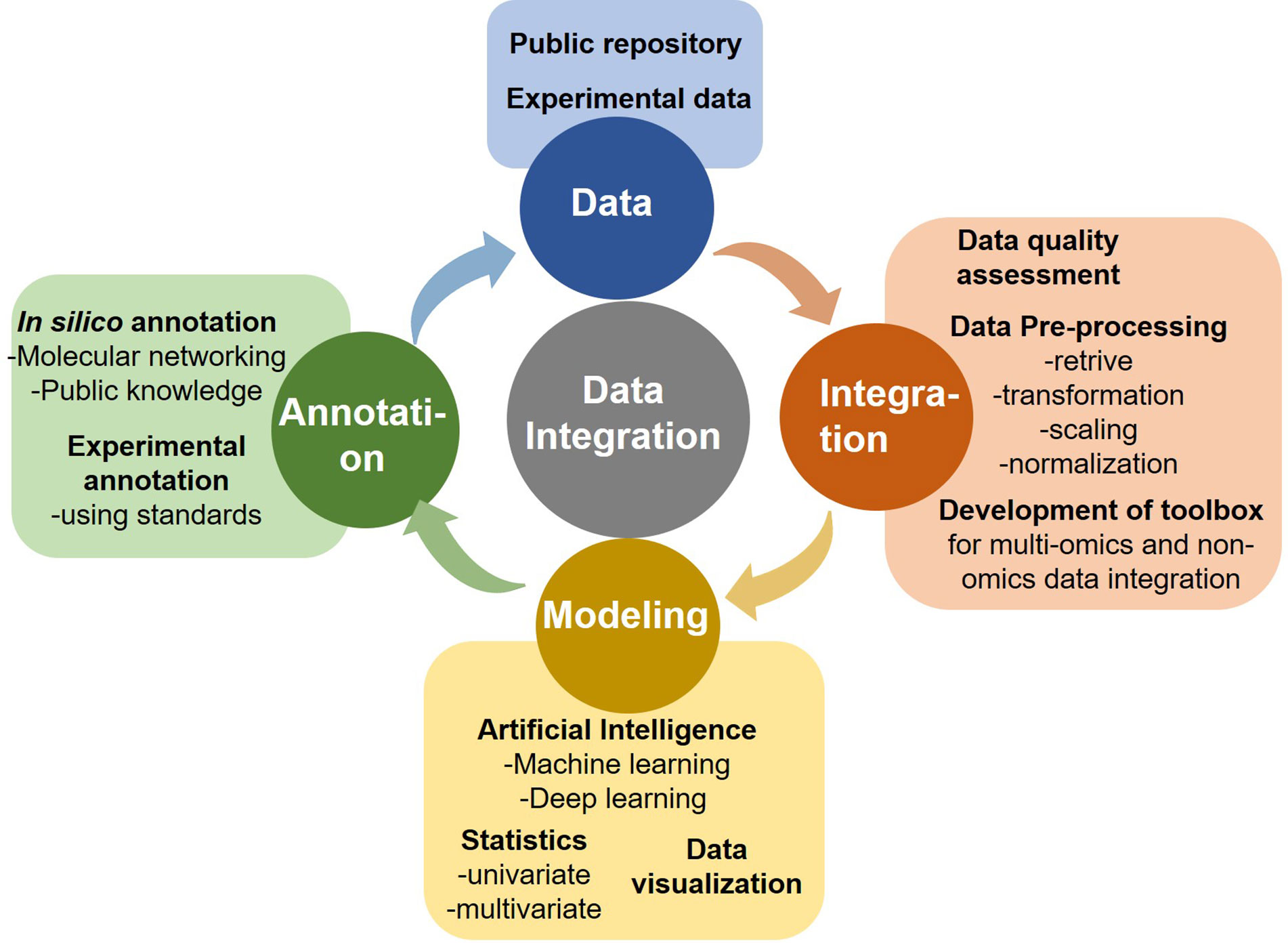
The integration of machine learning techniques has opened new avenues in cancer recurrence prediction, particularly for pediatric gliomas. Researchers are now employing sophisticated algorithms that utilize temporal learning — a method designed to analyze a series of MRI scans over time rather than isolated images. This approach allows the AI to detect subtle changes that may indicate the onset of recurrence, something traditional imaging methods might miss. In this regard, machine learning not only enhances diagnostic accuracy but also encourages ongoing learning from new data, continuously refining the algorithm for future predictions.
A significant finding from the study shows that by using temporal learning, the AI model achieved a prediction accuracy of between 75% and 89%, a remarkable improvement over single-image analysis that hovered around 50%. By learning from a sequence of images, the model becomes capable of recognizing patterns and deviations, providing a comprehensive understanding of a patient’s status over time. This leap in machine learning capability is essential as clinicians aim to make more informed, data-driven decisions regarding treatment plans and follow-up protocols.
As machine learning continues to evolve, the prospects for improving accuracy in cancer diagnosis and treatment planning only get brighter. With further validation and clinical application, AI can transform how we approach pediatric cancer care.
The Role of MRI Temporal Learning in Pediatric Oncology
MRI temporal learning represents a pioneering step in the field of pediatric oncology, particularly in the management of brain tumors. This innovative technique involves training AI models on multiple MRI scans that illustrate a patient’s progress over time, providing a temporal context that enhances the interpretative power of the scans. Unlike traditional methods that rely on individual images, temporal learning allows the algorithm to analyze changes from one scan to the next, offering insights into how a tumor evolves post-treatment.
By employing MRI temporal learning in pediatric cancer patients with gliomas, researchers at Mass General Brigham have created a tool that yields remarkably high predictive accuracy for tumor recurrence. This advancement is not merely a technical achievement; it has profound implications for clinical practice, enabling more timely interventions and potentially improving patient outcomes in a population that requires particularly sensitive care. As the technology and methodologies for developing these models continue to improve, the impact on pediatric oncology could be immense.
Enhancing Brain Cancer Accuracy with AI Technologies
In recent years, the accuracy of brain cancer predictions has seen remarkable improvements attributed to innovative AI technologies. Utilizing algorithms designed for medical imaging, researchers are better equipped to analyze complex datasets, leading to enhanced understanding of glioma behaviors and recurrence patterns. This improved accuracy is critical for tailoring treatment approaches to the specific needs of pediatric patients, ultimately aiming to minimize the long-term impact of their treatment procedures.
One of the notable innovations is the ability of AI systems to integrate diverse data sources from imaging scans. By synthesizing results from various time points, the AI can scrutinize changes in brain tumors from multiple angles. The result is a more holistic view that replaces the piecemeal approach of past methodologies. This improvement in brain cancer accuracy means clinicians can make more informed decisions regarding follow-ups and treatment adjustments, directly benefiting the children affected by these challenging conditions.
Looking Ahead: Clinical Trials and AI in Pediatric Cancer Treatment
As research progresses, there is growing excitement about the potential for AI-informed risk predictions to transform pediatric cancer treatment in clinical settings. The promising results from studies like those at Mass General Brigham indicate that AI tools can significantly alter the frequency and type of interventions required for pediatric patients, especially those at lower risk for recurrence. Looking ahead, clinical trials will be essential to evaluate the effectiveness of these AI models in real-world scenarios.
Incorporating AI into clinical trials is not just about improving accuracy in prediction; it has the potential to alter the entire landscape of pediatric oncology care. By identifying high-risk patients sooner, targeted adjuvant therapies could be applied preemptively, providing more systematic management of their treatment journey. Overall, the roadmap ahead is filled with opportunities to enhance care through the strategic application of advanced AI technologies in pediatric cancer management.
Implications of Research Funding for Pediatric Cancer Innovations
Financial investment in pediatric cancer research is vital for fostering innovations in diagnosis and treatment. With organizations like the National Institutes of Health supporting promising research projects, the future of pediatric oncology relies heavily on sustained funding that allows researchers to explore the capabilities of AI technologies. These investments not only empower researchers to develop more effective predictive models but also pave the way for transformative changes in clinical practices.
In particular, the collaboration between major hospitals and research institutions illustrates a unified approach toward tackling the unique challenges posed by pediatric cancers. The fusion of AI capabilities with robust research funding facilitates a culture of innovation that addresses urgent medical needs. Without these crucial investments, breakthroughs like the ones seen with MRI temporal learning and machine learning applications may take longer to materialize, ultimately affecting patient outcomes in the pediatric cancer realm.
Implementing AI: Challenges and Opportunities
While the advancements in AI technology for pediatric cancer treatment are promising, implementing such innovations poses its own set of challenges. Training AI models requires extensive and diverse datasets, which can be particularly difficult to amass in pediatric populations due to the rarity of certain tumors. Moreover, healthcare providers must ensure that these technologies are integrated seamlessly into existing workflows to enhance rather than hinder patient care.
However, these challenges also present opportunities for growth and collaboration among healthcare institutions. By working together to compile comprehensive datasets and sharing insights, hospitals can drive forward the capabilities of AI in pediatric oncology. The potential for collaborative projects can foster additional breakthroughs that not only improve predictive capabilities but also lead to enhanced, personalized care for pediatric patients suffering from cancer.
The Future of Pediatric Cancer AI: What Lies Ahead
The future of AI in pediatric cancer care is bright, with ongoing research and clinical trials poised to reshape how we approach diagnosis and treatment. As new technologies and methodologies are developed, we can expect continuous improvement in the accuracy of predictions for conditions like glioma, benefitting both patients and healthcare providers. The ongoing application of AI will likely pave the way for more preventive care practices, focused on early detection and timely intervention.
Moreover, as AI continues to demonstrate its capability to learn from an ever-expanding pool of data, we may witness an evolution in the way pediatric oncology is practiced. With advancements in monitoring tools and treatment protocols informed by AI insights, families dealing with pediatric cancer may experience less uncertainty and better outcomes. The journey toward integrating AI into pediatric cancer care is just beginning, but the potential for optimized treatment strategies is enormous.
Community Engagement in Pediatric Cancer Research
Community engagement plays a crucial role in advancing research and treatment options for pediatric cancer. By involving families, healthcare professionals, and advocacy groups in conversations about the importance of AI technologies, we can cultivate a supportive environment that emphasizes the need for participation in clinical trials and research initiatives. Such engagement ensures that research remains patient-centered, aligning scientific efforts with the actual needs and concerns of affected families.
Furthermore, a community-oriented approach can help to raise awareness of the potential benefits of AI in pediatric cancer prediction, making it easier for families to understand and trust emerging technologies. Community support can lead to more robust research funding and resource mobilization, ultimately improving care pathways for young patients diagnosed with cancer. As pediatric oncology continues to evolve, fostering strong ties between the research community and families is essential for maximizing the impact of innovations like AI.
Frequently Asked Questions
How is AI in pediatric cancer prediction improving glioma recurrence predictions?
AI in pediatric cancer prediction utilizes advanced machine learning techniques to analyze multiple MRI scans taken over time, significantly improving the accuracy in predicting glioma recurrence. The integration of temporal learning allows AI tools to recognize subtle changes in brain scans, leading to more precise assessments of relapse risks.
What role does machine learning play in pediatric cancer AI applications?
Machine learning is central to pediatric cancer AI applications, particularly in analyzing data from various imaging techniques. In predicting glioma recurrence, machine learning algorithms can process thousands of MRI scans to identify patterns and correlations, enhancing prediction accuracy compared to traditional methods, which often rely on single image interpretations.
Can MRI temporal learning enhance brain cancer prediction accuracy in children?
Yes, MRI temporal learning significantly enhances brain cancer prediction accuracy in children. By evaluating a series of MRI images taken over months, AI models can learn the progression of disease more effectively, achieving predictive accuracies of 75-89% for glioma recurrence, thus improving patient management strategies.
What advancements have been made in AI tools for pediatric glioma recurrence prediction?
Recent advancements in AI tools for pediatric glioma recurrence prediction include the implementation of temporal learning techniques that analyze sequential MRI scans. This innovative approach has been shown to outperform traditional methods, enabling clinicians to better identify children at high risk for relapse and optimize their treatment plans.
How does AI improve the management of pediatric brain cancer patients?
AI enhances the management of pediatric brain cancer patients by providing more accurate predictions of cancer recurrence. This allows for tailored follow-up care, potentially reducing unnecessary imaging for low-risk patients and ensuring timely intervention for those identified as high-risk through powerful machine learning and MRI analysis.
What is the significance of the study published in The New England Journal of Medicine AI regarding pediatric cancer?
The study published in The New England Journal of Medicine AI underscores the transformative potential of AI in pediatric cancer prediction, particularly for glioma recurrence. It demonstrates that by leveraging machine learning and temporal learning, researchers can achieve significant improvements in predictive accuracy, ultimately aiming to enhance patient care and treatment outcomes.
What is the potential impact of AI on the frequency of imaging for pediatric cancer?
AI has the potential to greatly impact the frequency of imaging for pediatric cancer patients. By accurately identifying low-risk patients, AI could reduce the need for frequent MRI scans, minimizing the stress and burden on children and their families while ensuring that high-risk patients receive appropriate monitoring and intervention.
What are the next steps for the research on AI in pediatric cancer prediction?
The next steps for the research on AI in pediatric cancer prediction include validating the temporal learning model across different clinical settings and initiating clinical trials to assess the practical applications of AI-informed risk predictions in managing glioma recurrence and treatment strategies.
| Key Point | Details |
|---|---|
| AI Tool Development | An AI tool was developed to analyze multiple brain scans over time, improving accuracy in predicting pediatric cancer relapse. |
| Study Significance | The study indicates AI can predict recurrence of gliomas with 75-89% accuracy compared to 50% by traditional methods. |
| Temporal Learning Technique | Utilized a novel temporal learning technique that analyzes patients’ MRI scans sequentially for better prediction. |
| Future Applications | Potential to improve patient care by adjusting imaging frequency and treatment strategies based on risk assessment. |
| Research Collaboration | Study conducted by Mass General Brigham in partnership with Boston Children’s Hospital and Dana-Farber/Boston’s Cancer program. |
Summary
AI in pediatric cancer prediction is a groundbreaking advancement that showcases how artificial intelligence can enhance the accuracy of detecting relapse risks in children diagnosed with brain tumors like gliomas. This innovation signifies a major step forward in patient care, potentially leading to personalized treatment plans and reducing unnecessary stress for families during follow-up periods. By leveraging advanced temporal learning techniques, the study emphasizes the importance of comprehensive imaging over mere single-scan assessments, establishing a promising framework for future clinical applications. As research continues, the integration of AI in pediatric oncology looks poised to revolutionize therapeutic approaches, ensuring that children receive timely and appropriate care.